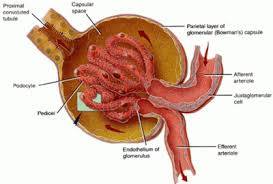
Acute glomerulonephritis (GN) comprises a specific set of renal diseases in which an immunologic mechanism triggers inflammation and proliferation of glomerular tissue that can result in damage to the basement membrane, mesangium, or capillary endothelium. Acute poststreptococcal glomerulonephritis (PSGN) is the archetype of acute GN. Acute nephritic syndrome is the most serious and potentially devastating form of the various renal syndromes.
Hippocrates originally described the natural history of acute GN, writing of back pain and hematuria followed by oliguria or anuria. Richard Bright described acute GN clinically in 1827, which led to the eponymic designation Bright disease. With the development of the microscope, Langhans was later able to describe these pathophysiologic glomerular changes.
Acute GN is defined as the sudden onset of hematuria, proteinuria, and red blood cell (RBC) casts. This clinical picture is often accompanied by hypertension, edema, azotemia (ie, decreased glomerular filtration rate [GFR]), and renal salt and water retention. Acute GN can be due to a primary renal disease or to a systemic disease. Most original research focuses on acute PSGN.
Treatment of PSGN is mainly supportive, because there is no specific therapy for renal disease. When acute GN is associated with chronic infections, the underlying infections must be treated. This article addresses the aspects of GN that are relevant to its acute management.
没有评论:
发表评论